Abstract
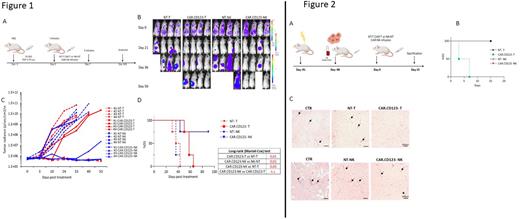
Paediatric Acute Myeloid Leukaemia (AML) is characterized by poor outcomes in patients with relapsed/refractory disease, despite the improvement of intensive standard therapy. Leukaemia cells of paediatric AML patients show a high expression of the CD123 antigen, this finding providing the biological basis to target CD123 with Chimeric Antigen Receptor (CAR). However, CAR.CD123 therapy in AML is hampered by on-target off-tumor toxicity, as well as by the long "vein-to-vein" time. In this scenario, we developed an off-the-shelf product based on allogeneic Natural Killer (NK) cells derived from peripheral blood of healthy donors, and engineered to express a second generation CAR.CD123 incorporating 4.1bb as costimulatory domain. CAR.CD123-NK cells showed significant in vitro anti-leukaemia activity not only against CD123+ AML cell lines, but also against CD123+ primary blasts (38,1%±4,8 NT-NK vs 3,6%±3,4 CAR-NK of CD123+ residual leukemic cells after 7-day co-culture; p<0.05). Moreover, the in vitro data were corroborated by an animal model of human AML-bearing immune-deficient mice. In particular, NSG mice were intravenously engrafted with CD123+ THP-1 cells genetically modified to express luciferase (Figure 1A). Mice showing leukemia engraftment were treated on Day 0 and 7 with effector cells (NT-T, CAR.CD123-T, NT-NK or CAR.CD123-NK cells). Bioluminescent imaging was used to measure the AML burden over time (1B). As expected, bioluminescence increased rapidly in mice treated with both controls NT-T and NT-NK cells (1B-C). Notably, CAR.CD123-NK cells induced a kinetics of leukemia control similar to that of CAR.CD123-T cells. These data were also corroborated by the overall survival (OS) analysis of the mice in each of the considered cohorts (1D). Remarkably, no difference was observed in the OS of mice treated with either CAR.CD123-NK cells or CAR.CD123-T cells. Once the anti-leukemia activity of CAR.CD123 NK cells was proved, we moved to evaluate the comparative on-target off-tumor effect of CAR.CD123 T and NK cells. We engrafted human haematopoietic cells from cord blood in an immune-deficient mouse model (hGM-CSF/hIL3 NOG genetically modified to express human GM-CSF and IL-3 cytokines). Ten weeks post-transplantation, mice were infused with either CAR.CD123-T, CAR.CD123-NK or un-modified T or NK cells (Fig. 2A). Five days after injection of effectors cells, all mice infused with CAR.CD123-T cells were dead, developing acute toxicity; by contrast, treatment with CAR.CD123-NK cells was not associated to toxicity as shown by OS data with 100% of the mice surviving at the Day 15, end of experiment (Fig. 2B). Lastly, it has been previously reported that CD123 antigen is expressed on endothelial cells and that these latter are specifically recognized and lysed by CAR.CD123-T cells. In light of these findings, we sought to define the toxicity profile of CAR.CD123 cells in a comprehensive animal model in which we developed a human endothelial tissue.
We engrafted the endothelial model in NSG mice, to test the safety profile of effector T and NK cells that have been infused after 2 weeks from the implant of human endothelial cells. Animals were sacrificed to collect the transplanted endothelium (Fig. 2C). Whereas the controls developed a dense network of vessels, as assessed by Haematoxylin/Eosin staining and counts of vessels/mm2 number, we observed a significant reduction of the number of vessels per mm2 in mice receiving CAR.CD123-T cells (p=0,001). In contrast, we did not observe any difference in terms of vessels/mm2 number in mice treated with CAR.CD123-NK cells or NT-NK cells.
Overall, our data indicate the feasibility of an innovative ''off-the-shelf'' therapeutic strategy based on CAR.CD123-NK cells, characterized by remarkable efficacy and improved safety profile as compared to CAR.CD123-T cells.
Disclosures
Locatelli:SOBI: Speakers Bureau; BLUEBIRD BIO: Speakers Bureau; TAKEDA: Speakers Bureau; GILEAD: Speakers Bureau; MEDAC: Speakers Bureau; MILTENYI: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; SANOFI: Membership on an entity's Board of Directors or advisory committees; NOVARTIS: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; NEOVII: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; AMGEN: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; PFIZER: Membership on an entity's Board of Directors or advisory committees; JAZZ PHARMACEUTICALS: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.